Exploring the Complexities of the Neuroscience of Addiction: How the Brain Shapes Behaviors and Choices
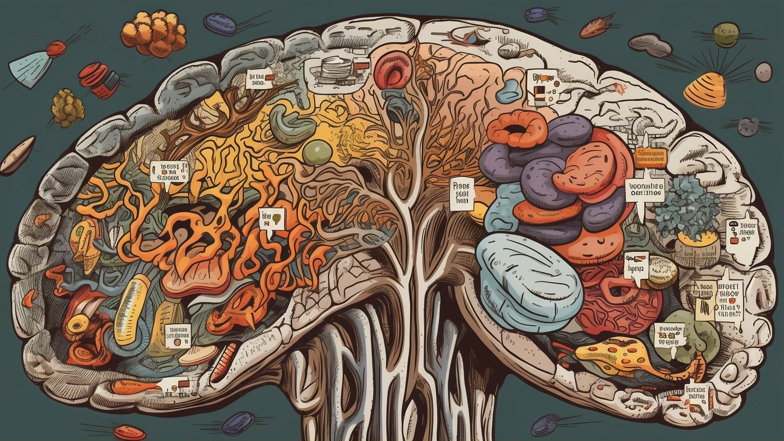
Addiction is a complex phenomenon that has long confounded scientists and laypeople alike. It is a multi-faceted, multi-layered condition that affects millions of people, regardless of age, race, or gender, and it is characterized by an individual's compulsive need to engage in a particular behavior, despite its negative consequences. Many scientists argue that addiction is primarily a brain disease, resulting from the complex interplay of various biological, genetic, and environmental factors. Understanding the neuroscience of addiction, therefore, requires an in-depth exploration of the mechanisms that underlie this condition, including the complex network of neural pathways that drive addiction-related behaviors and choices.
In this article, we will explore the neuroscience of addiction, its underlying mechanisms, and how these mechanisms shape behaviors and choices. Drawing on the latest research in this field, we will examine the role of various neurochemicals, neural circuits, and other neural structures in the development and maintenance of addiction, as well as the ways in which genetics, stress, and environmental factors influence this process. Finally, we will discuss some of the current treatments and therapies that are available for addiction and the challenges that researchers face in developing new and more effective treatments.
The Neurochemistry of Addiction
Neurochemistry is the study of how chemicals in the brain (neurotransmitters, hormones, and other signaling molecules) affect neural function and behavior. Many of the drugs that people become addicted to, such as cocaine or heroin, exert their effects by altering the activity of certain neurotransmitters in the brain. For example, cocaine increases the levels of dopamine in the brain, a neurotransmitter that is associated with feelings of pleasure and reward. This increase in dopamine levels leads to the euphoric rush that people experience when taking the drug, which can eventually lead to addiction when the drug is taken repeatedly or in high doses.
Other drugs, such as alcohol or marijuana, affect other neurotransmitters, such as GABA or endocannabinoids, which can also play a role in addiction. Over time, the brain adapts to these changes in neurotransmitter activity, becoming increasingly tolerant to the drug's effects and requiring more of the drug to achieve the same level of euphoria or to avoid negative withdrawal symptoms when the drug is no longer taken.
In addition to drugs, other behaviors, such as gambling, sex, or even social media use, can also activate the brain's reward system and lead to addiction-like behaviors. These behaviors can also be characterized by changes in neurotransmitter activity, with dopamine playing a prominent role in many cases. For example, when someone wins a game of chance and receives a reward, such as money or social recognition, dopamine is released in the brain, reinforcing the behavior that led to the reward and increasing the likelihood that the behavior will be repeated in the future.
Thus, the neurochemistry of addiction is characterized by a complex interplay between the brain's reward system and the effects of drugs or behaviors on neurotransmitter function. However, researchers are still trying to fully understand the intricacies of this process, including how changes in neurotransmitter activity relate to the development and persistence of addiction.
The Neural Circuits of Addiction
Neural circuits are the pathways that connect different brain regions and allow them to communicate with each other. These circuits can play a crucial role in addiction, influencing the way that the brain processes information related to reward and motivation, as well as the way that the brain responds to drugs or other reinforcing stimuli.
One of the key circuits involved in addiction is the mesolimbic pathway, which is involved in the processing of reward and motivation. This pathway originates in the ventral tegmental area (VTA), a small area in the midbrain that contains dopamine-producing neurons. These neurons project to various areas of the brain, including the nucleus accumbens, a region that is involved in the processing of reward and reinforcement.
When someone takes a drug or engages in a behavior that activates the reward system, such as winning a game of chance or receiving a compliment, dopamine is released from the VTA neurons and travels to the nucleus accumbens, where it binds to dopamine receptors and reinforces the behavior that led to the reward. This reinforcement can lead to the development of addiction over time, as the brain adapts to the increased dopamine levels and becomes increasingly tolerant to the drug or behavior.
Another important circuit involved in addiction is the prefrontal cortex (PFC), a region of the brain that is involved in decision-making, self-control, and other executive functions. The PFC is interconnected with the mesolimbic pathway, and this interaction is thought to play a crucial role in the regulation of addiction-related behavior. For example, the PFC can inhibit or modulate the activity of the mesolimbic pathway, helping to regulate the brain's response to drugs or other reinforcing stimuli. However, chronic drug use or other addictive behaviors can impair PFC function, leading to a breakdown in self-control and an increased likelihood of addiction-related behaviors.
Beyond these circuits, other brain regions and pathways are also thought to be involved in addiction, including the amygdala, hippocampus, and basal ganglia. These regions are involved in various processes related to emotion, memory, and motor control, and they can play a role in the way that the brain processes information related to addiction. However, the precise role of these regions in addiction is still being studied, and further research is needed to fully understand their contribution to this complex phenomenon.
Genetics, Stress, and Environmental Factors in Addiction
While the neurochemistry and neural circuits of addiction are crucial to understanding the development and maintenance of this condition, other factors also play a role. Genetics, stress, and environmental factors are all thought to influence the likelihood of addiction, as well as the way that addiction-related behaviors manifest.
Genetics is known to play a strong role in addiction, as certain genetic variations can increase the likelihood of addiction-related behaviors or make an individual more susceptible to the effects of drugs or other reinforcing stimuli. For example, variations in the DRD2 gene, which is involved in dopamine signaling, have been linked to an increased risk of addiction, particularly in individuals who have experienced early-life stress or trauma. Other genes, such as those involved in the development of GABA or endocannabinoid systems, have also been implicated in addiction susceptibility.
Stress is another factor that can influence the development and persistence of addiction. Chronic stress, such as that experienced by individuals who have experienced trauma or abuse, can lead to changes in the way that the brain processes reward and motivation, increasing the likelihood of addiction-related behaviors. Stress can also contribute to the development of co-occurring mental health conditions, such as depression or anxiety, which can further increase the risk of addiction.
Finally, environmental factors, such as exposure to drugs or alcohol, can also play a role in the development of addiction. Individuals who grow up in environments where drugs or alcohol are readily available may be more likely to develop addiction-related behaviors, particularly if they also experience stress or trauma. Furthermore, exposure to drugs or other reinforcing stimuli during early development can lead to changes in the neural circuits involved in addiction, making an individual more susceptible to addiction-related behaviors in the future.
Treatment and Future Directions
While addiction is a complex and multifaceted condition, there are various treatments and therapies available to help individuals recover from addiction and regain control over their lives. These treatments include behavioral therapies, such as Cognitive Behavioral Therapy (CBT), which can help individuals identify and change addiction-related behaviors, as well as pharmacological treatments, such as methadone or buprenorphine, which can help to alleviate withdrawal symptoms and reduce drug cravings.
However, there are still challenges in the treatment of addiction, including the development of new and more effective treatments, as well as the recognition of addiction as a chronic and relapsing disease. Additionally, the stigma surrounding addiction can make it more difficult for individuals to seek treatment, particularly in settings where addiction is viewed as a moral failing rather than a medical condition.
Future research in the field of addiction neuroscience will likely focus on identifying new targets for pharmacological interventions, as well as developing new behavioral therapies that can help individuals overcome addiction-related behaviors and regain control over their lives. Furthermore, as our understanding of the genetic and environmental factors that contribute to addiction continues to grow, researchers may be better able to develop personalized treatments that can target the underlying causes of addiction in individual patients.
Conclusion
Addiction is a complex and multifaceted condition that is characterized by compulsive behaviors and choices, despite their negative consequences. Understanding the neuroscience of addiction requires an exploration of the various mechanisms that underlie this condition, including the role of neurochemistry, neural circuits, genetics, stress, and environmental factors. While many treatments and therapies are available to help individuals overcome addiction-related behaviors, further research is needed to fully understand the intricacies of this condition and to develop new and more effective treatments in the future.
Comments
Post a Comment